Emergency service call takers under extreme stress, with little support
By Nick Watts
A US study conducted by Dr Michelle Lilly from Northern Illinois University shows a strong link between the 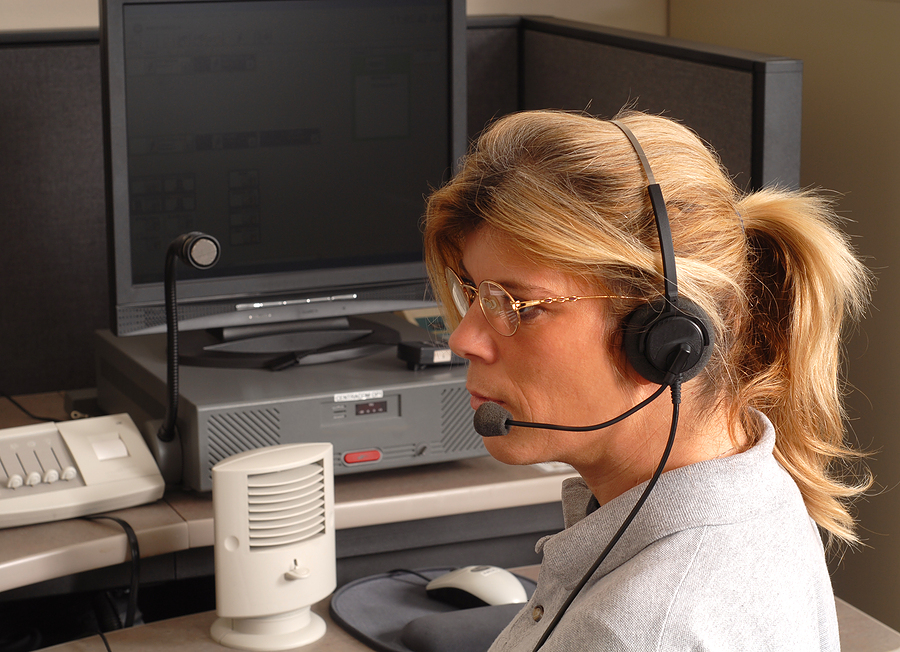 people who answer emergency calls and the development of PTSD following traumatic calls. They rated the death of serious injury of a child as the most traumatic call they could deal with, closely followed by suicidal callers, shootings involving police officers and the unexpected death of an adult.
people who answer emergency calls and the development of PTSD following traumatic calls. They rated the death of serious injury of a child as the most traumatic call they could deal with, closely followed by suicidal callers, shootings involving police officers and the unexpected death of an adult.
The research indicates that many call takers report symptoms of severe stress and a further 3.5% reporting symptoms serious enough to be diagnosed with Post Traumatic Stress Disorder. This research goes to prove that direct exposure to traumatic events is not necessary to lead to serious issues with stress and PTSD.
I wanted to find out what it was like for UK emergency services and how they supported call takers who provide that vital initial response to every incident. I spoke with an emergency call taker for South Central Ambulance Service, who describes a “lack of support available to control staff”;
“Traumatic calls are incredibly difficult to deal with as you try to calm people down so you can help, this is frustrating as you can only do as much as the caller allows. The hardest thing about it is the lack of closure as you do your bit in the whole process and rarely find out the outcome”
He was telling me that he knows many call takers who have been signed off work with stress, including himself and several who have left because “it became too much to handle”. When I asked what kind of calls are among the worst the answer echoed with the research, he also told me about the most traumatic event he had to deal with;
“Anything involving children is the worst, it is hard to get the caller to calm down enough to be able to help and get the right information. My most traumatic call involved a baby and it really shook me, yet due to staff shortages I had to continue to answer calls even though I felt unable to.”
The last bit worried me, how can you do your job effectively under such stress? So we went on to talk a little bit more about the support they receive;
“There is a lack of support available to us, with no internal support network and all that is available to us is a private company. Many of us feel this is inappropriate because they have no real understanding of the needs and difficulties faced by emergency call taking staff. Very occasionally you will take part in a big debriefing, but this has only happened to me twice in 5 years, usually you just get your manager telling you to ‘go get a cuppa’.
It is clear that there is a lack of support available to them, at a time when they need it the most. To have to continue to take calls following such a traumatic event not only harms the call taker, but likely reduces their effectiveness, potentially placing the public at risk. It is also clear that many get signed off with stress related issues, when if there was an internal support structure they may be able to deal with the difficult situation more effectively, reducing the level of distress felt by these workers. South Central Ambulance Service responded with this statement;
“999 call takers work on the frontline of the emergency response process. Theirs is a critical role, and as such can be stressful. South Central Ambulance Service NHS Foundation Trust ensures we have robust support mechanisms for our staff. Managers are trained to identify traumatised or stressed staff and provide them with support. Staff can also access confidential support from an external counselling service, PPC, full details of which are available to staff.”
All in all, call takers feel undervalued and unable to seek support, with the one I interviewed commenting that they were treated differently to ‘frontline’ staff;
“They are stood down from duty, debriefed and is necessary sent home.”
Dr Michelle Lilly’s findings were similar during her research study acknowledging the need for preventative work to be done alongside intervention where necessary with staff that is currently only provided for ‘frontline’ colleagues.





